Pubovaginal Sling (rectus fascial sling)
Rectus fascia sling (also known as pubovaginal sling or autologous sling) is an operation to treat stress urinary incontinence. Stress incontinence is leakage of urine that occurs with activities which cause an increase in abdominal pressure such as coughing, sneezing, jumping, lifting, exercising and in some cases walking.
This leakage occurs because the muscles at the bladder neck have lost their supports and strength. As a valve mechanism, the urethra (waterpipe) no longer stays closed when extra pressure is put on the bladder.
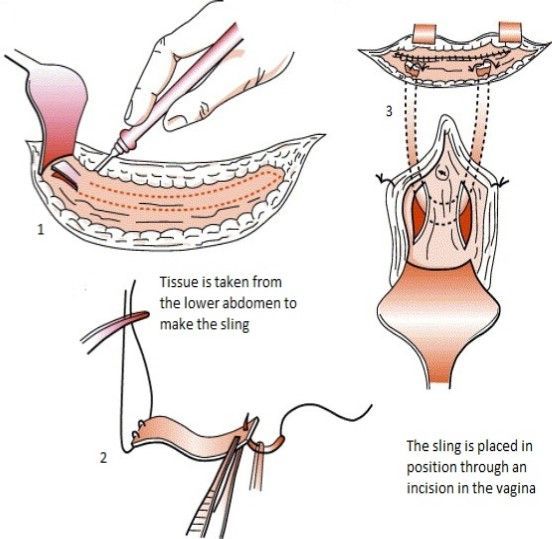
In this operation a strip of tissue is taken from the lower abdomen (tummy) and used as a sling or hammock around the bladder neck and urethra. This differs to other types of sling such as the TVT sling, which uses a synthetic material/mesh to create the sling. The rectus fascia sling therefore provides a mesh-free alternative.
The rectus fascia is the thin but very tough layer that covers the abdominal muscles. A small incision is made just below the bikini line and a strip of the rectus fascia is removed. It is then placed in position under the urethra through an incision in the vagina as a supportive sling.
On average most women are in hospital 2 nights following this type of surgery.
Before your operation
In the weeks just prior to surgery it is common to come to Urology Associates to see the continence nurse specialist for a pre-op appointment.
You may have a routine blood test and a urine sample taken prior to your operation.
The operation and outcomes will be explained to you by your Urologist. When you feel comfortable that you understand what is to be done and have had all your questions answered you will be asked to sign a consent form.
It is important to avoid constipation. Try to establish and maintain a regular, soft bowel habit leading up to your operation. Identify the foods that can help you in this area for your post-op period.
Operation day
You will be advised when to come to hospital (usually by phone the day before your operation).
It is usual to stop eating and drinking at least 6 hours prior to surgery. You should bring your own medications with you and the staff will advise you if you need to take them on the day of your operation.
Before the operation you will be given supportive stockings to wear until you leave hospital to minimise the risk of blood clots forming.
Whether you have a spinal or general anaesthetic will be decided after discussion with the anaesthetist. This usually occurs during in the ward pre-operatively. Just prior to surgery you may be given a pre-medication tablet to relax you.
You will be encouraged to commence deep breathing and coughing exercises to prevent any breathing complications or chest infection occurring following the surgery and anaesthetic.
Recovery
There will be a light dressing on your lower abdomen over the incision.
You will have a catheter (tube) in your bladder via your urethra, draining your urine into a bag.
While in hospital you will be prescribed paracetamol and you should take this regularly to keep any discomfort to a minimum. Ask the nurses for stronger pain relief if needed.
If a gauze pack was placed in the vagina during surgery, it will usually be removed the next morning before your shower.
One you are drinking normally and your pain is controlled, your drip will be removed.
Catheter
- This will usually be removed after two days.
- After a normal intake of fluid it is usual to pass urine every 3-4 hours.
- Initially you should not wait longer than this time before trying to empty your bladder.
- You may find emptying your bladder feels different as it recovers from the surgery and the associated swelling of the surrounding tissues.
- Try to relax your abdominal muscles and the muscles underneath your bladder. Take your time and just let the urine flow out. Do not push or strain as this forces the urethra against the sling, closing it off and stopping the flow of urine.
It is common not to be able to pass urine afterwards. If you cannot pass urine, can pass only a small amount or have bladder discomfort please let your nurse know. The nurse may check your residual urine and arrange a self-catheterisation program if needed. This is called Clean Intermittent Catheterisation (CIC) and can be performed in the privacy of your own bathroom or any toilet. Initially you may have to catheterise each time you need to pass urine but as things return to normal the frequency of your CIC will be reduced. It is not expected that you will need to do this in the long-term unless your urologist advises you of this before the operation.
After discharge
Our nurses will contact you by phone to check on your progress. If you have any concerns you may ring any time or arrange an appointment. You will also have a follow-up consultation with your surgeon at approximately six weeks post surgery.
Bowels
Keeping a regular, soft bowel motion is important. Kiwi fruit or "Kiwi Crush" are also recommended.
Pain control
Take regular pain control. Paracetamol or anti-inflammatory medication such as diclofenac (Voltaren) or ibuprofen (Nurofen) are usually effective.
The more you do, the worse your abdominal pain will get. Use this as a guide for the amount of activity that you do over the next few weeks. If you are sore, rest.
Wound pain sometimes may be worse on one side than the other.
Wound care
Your abdominal incision and vaginal wound should heal within 7-10 days however the muscle layer beneath your skin will take up to 3 months to heal. The dressing tape can be removed after 7-10 days.
If you notice the incision becomes inflamed, there is an increase in pain, or it is red, hot or swollen, contact Urology Associates for advice.
Wound care
Your abdominal cuts and vaginal wound should heal within 7-10 days however the muscle layer beneath your skin will take up to 3 months to heal. The dressing tape can be removed after 7-10 days.
If you notice the cuts become inflamed, there is an increase in pain, or it is red, hot or swollen, contact Urology Associates for advice.
Vaginal discharge
It is normal to have some vaginal bleeding on and off for a few weeks and then a brown discharge for a few weeks following that. If the bleeding becomes heavy, you pass clots or have a smelly vaginal discharge, contact Urology Associates.
You may also notice the remains of some stitches in your underwear or in the toilet after emptying your bladder. Do not be concerned as these are vaginal stitches which have started to dissolve and that is expected.
Pelvic Floor Exercises
It is important to continue pelvic floor exercises once you have recovered from surgery. If you have any concerns about your technique, please contact our continence nurse specialist.
Activity
Initially when you go home you will not feel like doing very much, so listen to your body and rest. Sitting with your feet up will be the most comfortable position.
Things you can do include:
- Showering
- Preparing light meals
- Walking up and down stairs slowly
- Gentle walking is to be encouraged – it is better to do two short walks in the day rather than one long walk
Things you should not do for 6 weeks include:
- Picking up heavy objects off the floor
- Housework except light work at bench height
- Vacuuming
- Carrying supermarket bags / rubbish bags
- Carrying children / pets
Things that you should not do for 12 weeks include:
- Heavy lifting
- Shifting the furniture
- Lawn mowing or digging the garden
- Weights at the gym
- Carrying rubbish bags or washing baskets
- Carrying children / pets
Driving
You should not drive until you feel that you could perform an emergency stop without being concerned about abdominal pain (approximately 3-4 weeks).
Returning to work
Ask your specialist about returning to work. This will vary according to the type of operation performed and whether you have a manual or sedentary occupation. Usually people are off work for about 4-6 weeks.
Sexual Intercourse
You can resume sexual intercourse at 6 weeks but some women may need to adopt alternative positions if they experience any discomfort. You can discuss this with your specialist.
Complications
Seek help from your GP or Urology Associates if you develop:
- Flu like symtoms
- A temperature over 38°C
- Pain or discomfort not controlled by pain medication
- Bleeding or difficulty passing urine
- Pain or tenderness in the calf or thigh
- Symptoms of a urinary tract infection such as pain on passing urine, going more often than usual or smelly urine.